An x-ray uses radiation to take pictures of the inside of the body.
What is an X-ray?
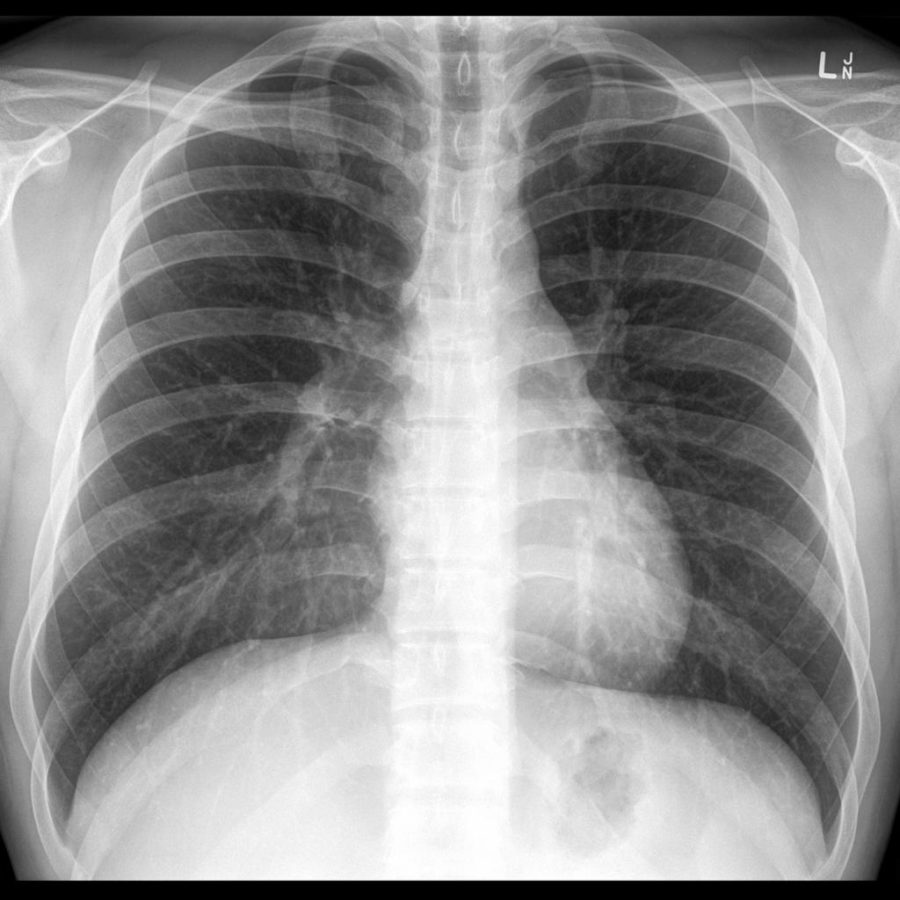
An x-ray uses radiation to take pictures of the inside of the body. The X-ray can show bones, soft tissue (e.g. muscle and fat) and fluid. The picture is created because the different structures in our body absorbs the radiation at different levels. On the scan:
- Bone appears as white
- Air (for example in the lungs) appears as black
- Muscle, fat and fluid appear as grey
What happens before the test?
There is no special preparation required. A gown will be given to you to wear and any jewellery or anything that is metal must be removed. It is important that staff are advised if there is a chance that you are pregnant. If there is, this will make a difference in the way that the X-rays are taken. Eating and drinking as normal is allowed and usual medications can be taken before an X-ray.
What happens during the test?
An X-ray is painless, and the process normally takes around 15 minutes. The procedure will be explained by the radiographer and the position you are put in e.g. lie, sit or stand depends on which part of the body is being X-rayed. It is important to be as comfortable as possible as staying still whilst the radiographer is taking the X-ray is very important.
What happens after the test?
The radiographer will check the images to make sure they are good quality and, in some cases, they may need to have additional X-rays taken if the radiographer needs a better image. This is a normal procedure and nothing to worry about. Once the images have been checked you will be able to go home. The radiologist will review the x-rays and write a report, which is sent to the doctor. You will need to follow up with the doctor who requested the X-ray, to get the results.
Are there any side effects or risks?
An X-ray will deliver a small amount of radiation and there is little or no evidence of health effects for this dose of radiation.
Before diagnosis, the GP or the haematologist may request an X-ray to detect a mass or abnormality in the body. This will often depend because of the symptoms being experienced and if the X-ray shows something suspicious, they will then order more tests. These can include an ultrasound, CT scan or PET scan.
Note: A biopsy is always needed for the diagnosis of lymphoma.