Having treatment for lymphoma is often a life-saving decision. However, it also puts you at greater risk of developing a second cancer later in life. In most cases a second cancer may occur more than 10 years after you start your lymphoma treatment. In very rare cases it may happen earlier.
A weakened immune system, chemotherapy and radiation therapy can all increase your risk of a second cancer that is different to your initial lymphoma. Other treatments may also increase your risk.
Not everyone who has had treatment will get a second cancer, but it’s important to be aware of the risk so you can manage your health and get medical advice early. Having regular checkups with your general practitioner (GP), haematologist, oncologist or radiation oncologist is an important part of making sure any second cancers are picked up early and treated when needed.
This page will provide information on what to look for, what checkups you should have, and when to see a doctor about new symptoms.
What is a second cancer
A second cancer is the development of a new cancer unrelated to your original lymphoma or CLL diagnosis. It is not a relapse or transformation of your lymphoma/CLL.
For more information on relapsed or transformed lymphoma, click the links below.
Why do second cancers happen?
Some treatments work by changing the way your immune system works, while others cause direct damage to the DNA of your cells. This is important because it helps to destroy the lymphoma cells. However, it can also increase your risk of second cancers as your immune system may be weakened, or DNA damage may eventually result in more rogue (damaged) cells escaping your immune system and multiplying until they become cancer.
Most people do not get a second cancer. However, it is important to know of your risk so you can have routine screening and get medical advice early.
How do cells normally grow?
Normally cells grow and multiply in a very tightly controlled and organised way. They are programmed to grow and behave in a certain way, and multiply or die at certain times.
Cells on their own are microscopic – meaning they are so small we can not see them. But, when they all join together they make up every part of our body including our skin, nails, bones, hair, lymph nodes, blood and body organs.
There are many checks and balances that happen to make sure cells develop the right way. These include “immune checkpoints”. Immune checkpoints are points during the cell growth where our immune system “checks” that the cell is a normal, healthy cell.
If the cell is checked and found to be healthy, it continues to grow. If it is diseased, or damaged in some way, it is either repaired or destroyed (dies), and removed from our body through our lymphatic system.
- When cells multiply, it is called cell division.
- When cells die it is called apoptosis.
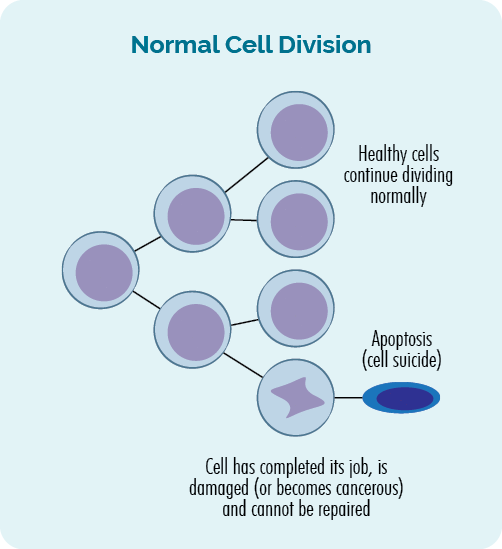
This process of cell division and apoptosis is regulated by the genes in our DNA, and is happening in our bodies all the time. We make trillions of cells every day to replace the old ones that have completed their job or become damaged.
Genes and DNA
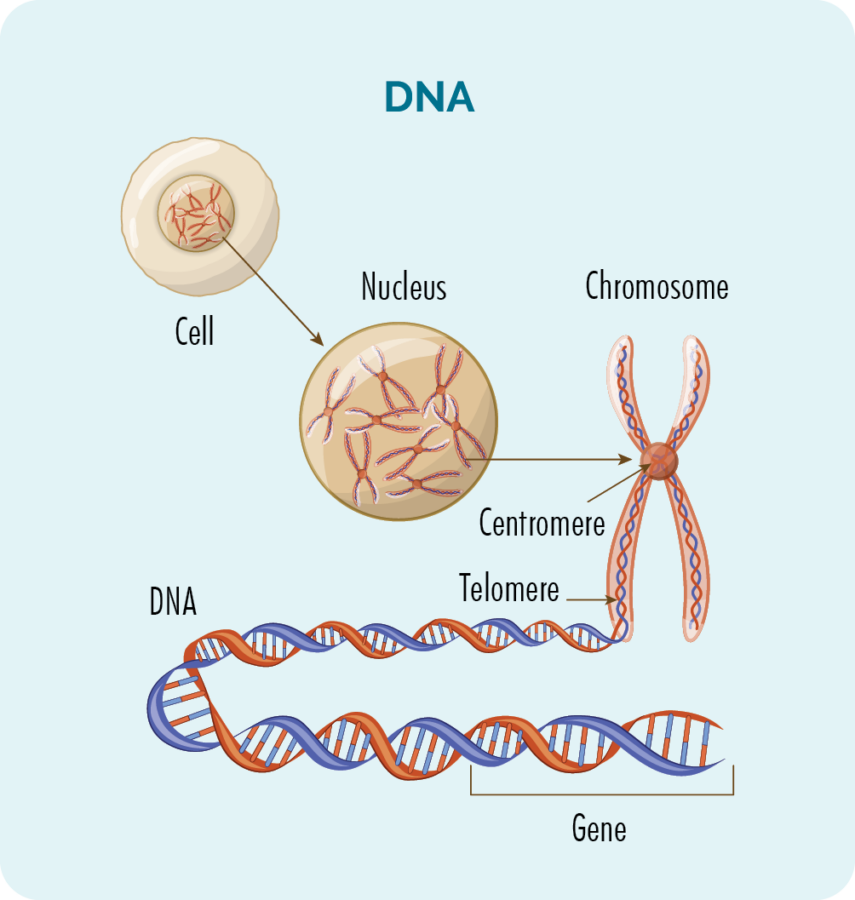
Inside every cell (except for red blood cells) is a nucleus with 23 pairs of chromosomes.
Chromosomes are made up of our DNA, and our DNA is made up of many different genes which provide the “recipe” for how our cells should grow, multiply, work and eventually die.
Cancer occurs when damage or mistakes happen in our genes. Some treatments for lymphoma can cause some lasting damage to the genes.
Learn more about what happens when our genes and DNA are damaged in the video below. Don’t worry too much about all the names of proteins and processes, the names are not as important as what they do.
What is cancer?
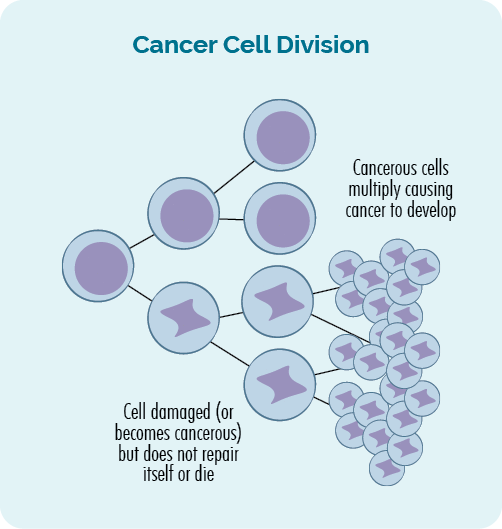
Cancer is a genetic disease. It occurs when damage or mistakes occur in our genes, resulting in abnormal, uncontrolled growth of cells.
Cancer happens when the uncontrolled and abnormal growth of cells continues and forms a tumour, or an increase in cancerous cells in your blood or lymphatic system.
These changes to our DNA are sometimes called genetic mutations or genetic variations.
Secondary cancers happen because of the damage treatment for your first cancer – lymphoma or CLL causes to your DNA, genes or immune system.
What type of secondary cancer can occur?
Having treatment for lymphoma can put you at a slightly higher risk of any type of cancer. However, the risk of certain second cancers may be higher dependent on the type of treatment you have, and the location of the lymphoma being treated.
Treatment with chemotherapy may increase your risk of a second blood cancer such as myeloma or leukemia or, if you have had Hodgkin Lymphoma, you may develop a subtype of Non-Hodgkin Lymphoma. Car T-cell therapy may increase your risk of developing a T-cell lymphoma, leukemia or skin cancer, though the risk is believed to be small.
The risk of a second cancer after radiation treatment is related to the area of your body where the radiation treatment was targeting.
Click on the headings below to learn more about the risk of the more common types of second cancers.
Skin cancers can be:
- Basal cell carcinomas
- Squamous cell carcinoma
- Melanomas
- Merkel cell carcinomas.
Breast cancer is more common in women than men, but men can still get breast cancer. If you have had radiation to your chest, you may be at increased risk of developing breast cancer later in life.
You should start having yearly checks such as mammogram and ultrasound from the age of 30 years, or 8 years after you start treatment for lymphoma/CLL – whichever comes first.
Your risk of developing breast cancer as a long-term effect of your lymphoma treatment is higher if you had radiation to your chest when you were less than 30 years of age.
Ask your GP (local doctor) to show you how to check your breasts for lumps. Check for lumps monthly and report any changes to your GP.
You may develop a second and unrelated lymphoma. This is different to a relapse or transformed lymphoma.
For example, if you have previously had treatment for Hodgkin Lymphoma, you may develop a second lymphoma which is a subtype of Non-Hodgkin Lymphoma (NHL). If you’ve had NHL in the past, you may develop a different type of NHL or Hodgkin Lymphoma.
Some people have developed a T-cell lymphoma after CAR T-cell therapy for a B-cell lymphoma.
Click here from more information on symptoms of lymphoma and when to see your doctor.
Depending on the type of treatment you had, you may be at increased risk of developing a type leukemia called Acute Myeloid Leukemia (AML). Symptoms of AML inlcude:
- Bleeding or bruising easier than usual, or purple or reddish spotty rash.
- Fatigue and general weakness
- Weight loss with or without loss of appetite
- Sores that don’t heal as expected
- Fever and/or chills
- Infections that keep coming back or don’t go away
- Difficulty breathing, shortness of breath or chest pain
- Changes in your blood tests.
Ask your doctor if you are at an increased risk of developing AML and what follow up you may need.
You may be at a slight increased risk of developing lung cancer later in life if you have had radiation to your chest. This risk is increased if you smoke, however even non-smokers may get it.
Newer techniques in radiation treatment are making it safer and decreasing the risk, but you should report any respiratory symptoms to your doctor if they last longer than two weeks. These include:
- Feeling short of breath for no reason
- Feeling tired or out of breath sooner than expected when you exercise
- Pain in your chest
- Discomfort when you breathe
- Coughing with or without phlegm
- Coughing up blood.
You may be at increased risk of developing thyroid cancer if you have had radiation to your neck or throat.
Symptoms of thyroid cancer include:
- Sore throat or pain in the front of your neck that may travel up to your ears
- A lump in the front of your throat
- Swelling in your neck
- Difficulty swallowing or breathing
- Changes to your voice
- A cough that does not go away.
See your local doctor (GP) if any of these symptoms are severe, or if they last longer than 2 weeks.
Radiation to your abdomen or bowels may increase your risk of developing bowel cancer later in life. Report all changes to your doctor for review. Changes you may get include:
- Diarrhea or constipation
- Bloating or pain in your abdomen and tummy
- Blood when you go to the toilet – this may look like bright red blood or a dark sticky black poo
- Difficulty eating due to feeling full
- Nausea and vomiting
- Weight loss without trying.
You may be at increased risk of prostate cancer if you have had radiation to your abdomen or pelvic area, or had other types of anti-cancer medicines such as chemo, targeted or immunotherapies.
Have regular prostate checks with your GP and report any changes such as:
- difficulty with urine flow (weeing) or needing to go more than usual
- changes in getting an erection or blood in your semen
- pain, bloating or discomfort in your abdomen.
What second cancers you may be at risk of, and what follow up tests and scans you should have. Your GP will be able to help to organise these tests.
Is it worth the risk of having treatment?
This is a very personal decision. The risk of developing a second cancer, though higher than for those who haven’t had treatment for lymphoma, is still low.
By having treatment now, you can hopefully achieve remission or even cure from your current lymphoma. This can possibly give you many more years of good quality life.
Knowing there is a risk of a second cancer may cause anxiety, but also means you know what symptoms to look out for and when to see a doctor. It also means you will be followed closely and have scans or tests done to pick up any potential second cancer early. This will hopefully give you the best chance of having it treated successfully.
However, only you can decide what risks you are willing to take with your health. Ask your haematologist questions about the risks of not having the treatment they recommend. Ask them about your risks of a second cancer and what follow up tests you should have.
Then, talk to your loved ones or a psychologist if you need to. Make your decision based on the information you have been given, and what is right for you. If you feel you haven’t got enough information, you can also ask for a second opinion on your treatment. Your haematologist or GP can help you arrange a second opinion.
What follow up tests should I have?
There is no specific protocol to do follow up testing for second cancers after treatment. This is because what you need will depend on the type of lymphoma you had, what treatments you had, and the areas of your body affected.
Talk to your haematologist or oncologist about the types of follow up tests you should have. However, below is guide to what you need to consider.
- Regular blood tests as recommended by your oncologist or haematologist.
- Monthly self-breast checks (report changes to your GP as soon as possible), and mammogram and/or ultrasound as recommended by your doctor.
- Yearly mammogram and ultrasound from age 30 years or 8 years after radiation to your chest if treatment was before the age of 30 years.
- Pap smears as recommended by your doctor.
- Yearly skin checks – more often if recommended by your doctor.
- Bowel screening every second year from age 50 years, and earlier if recommended by your doctor.
- Prostate checks yearly from age 50 years, and earlier if recommended by your doctor.
- Vaccinations as recommended by your doctor.
Summary
- Lymphoma treatments can be lifesaving, but all types of treatment also put you at a higher risk of getting a second cancer later in life.
- Second cancers are not a relapse or transformation of your original lymphoma. It is a different type of cancer unrelated to your lymphoma.
- Treatment with radiotherapy can put you at greater risk of a second cancer in the area where the radiation was directed.
- Chemotherapy can increase your risk of a second blood cancer, or other types of solid tumours.
- Skin cancers are the most common second cancer. Yearly skin checks are important.
- Men and women can both get breast cancer though it is more common in women. If you have had radiation to your chest, start doing monthly self-checks, and report all changes to your doctor.
- Keep up to date with all your recommended screening tests, scans, and vaccinations.
- Ask your haematologist, oncologist or radiation oncologist about your risks of second cancers and make a plan with them for follow up care.
- If you don’t already have GP you trust, look for one and let them know of your treatments and ongoing risks. Ask them to liaise with your haematologist, oncologist or radiation oncologists for guidance on ongoing follow up care.