This webpage is dedicated to patients and their carers living with lymphoma and CLL in regional, rural and remote (RRR) Australia. It aims to bridge the gap of resources and provide you with important information on how to get the right care at the right time. We will also provide information on how to get a diagnosis, how to care for yourself if you’re having treatment, and coordinating your care, before, during and after treatment, when faced with the additional challenges that RRR life brings.
The Australian Dream: Life and Healthcare Challenges in the Outback
For many, the Australian Dream is a life of wide-open spaces, close-knit communities, and a deep connection to the land. Living in regional, rural, and remote Australia offers a sense of freedom, self-sufficiency, and an escape from the pressures of city life. However, when disaster strikes—such as a cancer diagnosis—the idyllic dream can quickly become a logistical, financial and emotional nightmare.
Accessing the right care at the right time becomes an overwhelming challenge. Specialist cancer services are often hundreds, if not thousands, of kilometers away. Travel for treatment means time away from family, work, and community, adding financial and emotional strain.
Telehealth has improved access to consultations, but it cannot replace the need for in-person treatments such as chemotherapy, radiation, or surgery. Delays in diagnosis and treatment due to workforce shortages, limited facilities, and long wait times can drastically impact outcomes.
For many, the burden is not just medical but deeply personal—having to choose between staying close to home or relocating for life-saving care. The resilience of rural Australians is unmatched, but without significant improvements in healthcare accessibility, the gap between city and country treatment outcomes remains an unacceptable reality.
At Lymphoma Australia, we aim to do our part to bridge this gap by giving you access to vital information you need, to help you navigate the healthcare system, and your health effectively.
About Lymphoma
There are many resources you will find on this website about lymphoma, and to learn more, please see the links below. However, this webpage will look at the extra considerations you may have when you live in RRR Australia.
Getting a diagnosis
Many people report delays in getting a diagnosis of lymphoma even when they live close to, and have regular access to doctors and hospitals.
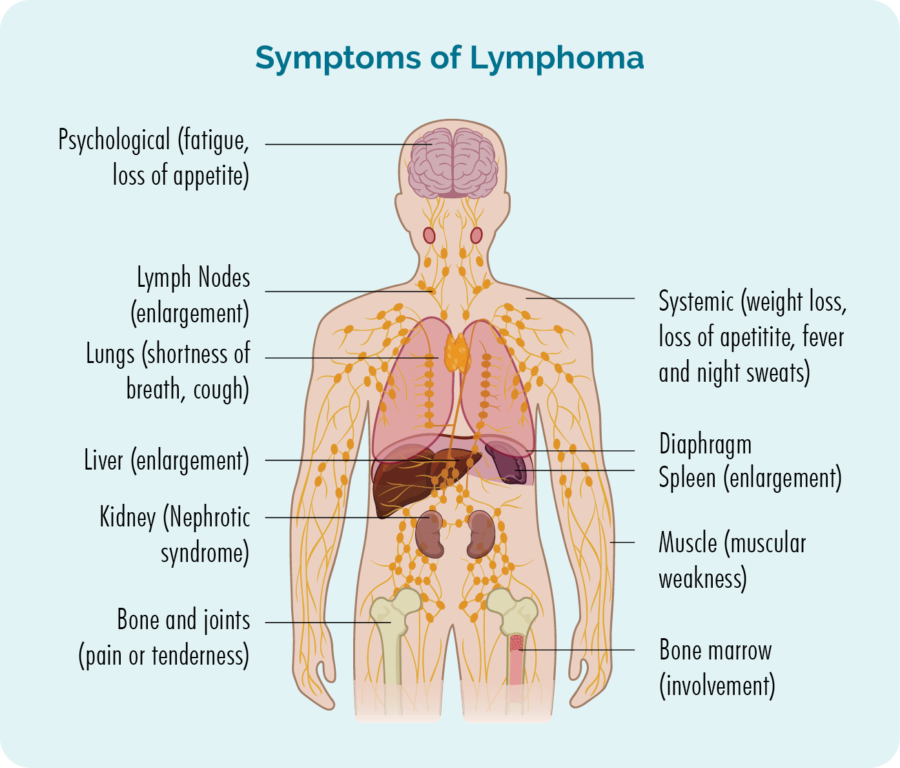
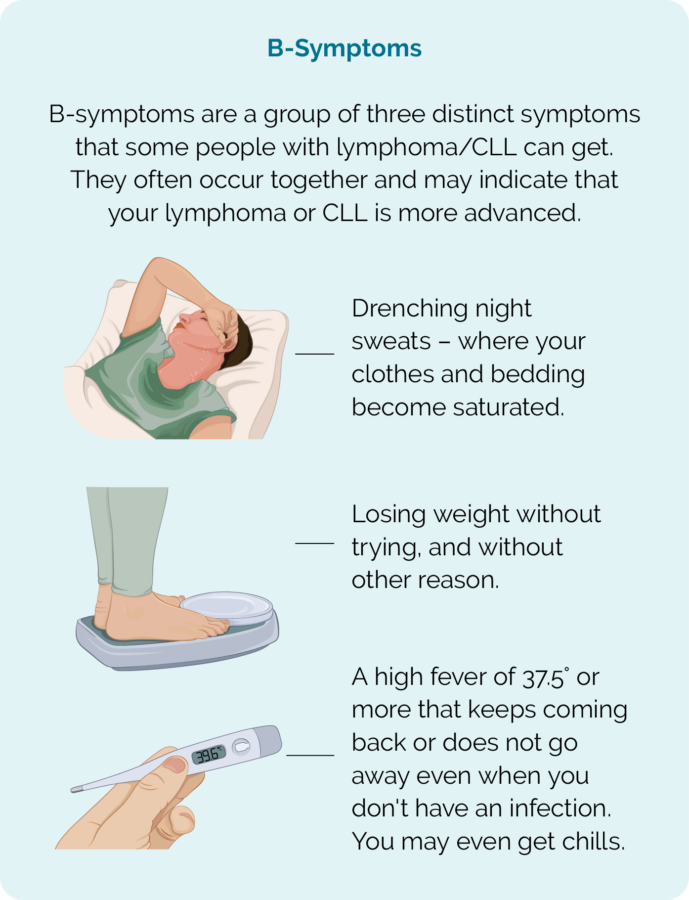
This is in large part because many symptoms of lymphoma mimic many other, more common conditions such as infections, allergies, iron deficiency and stress. Not only that, but even though lymphoma is a cancer of your blood cells (called lymphocytes), many people have completely normal blood tests, even though they have lymphoma. This is because unlike other blood cells, most of our lymphocytes live in our lymph nodes (glands) rather than in our blood.
Additionally, lymphoma can start in ANY part of your body, and with more than 80 different subtypes of lymphoma the symptoms you get, may be very different from the symptoms somebody else gets. And, many GPs have never cared for a patient with lymphoma, or your specific subtype of lymphoma.
The added challenge when living in RRR Australia

With all the benefits of RRR living, some of the biggest challenges you may face is access to healthcare services close to home.
Without a daily GP service nearby, and with healthcare staff often on short-term contracts, you may have delays seeing a doctor, getting tests and biopsies, and no continuity of care. Having the confidence to advocate for yourself, in these situations is crucial to making sure you get the right care.
Below are some tips you can use to take charge of your own health and ensure you get the care you need.
Keep your health information together
If you have a MyGov account, you can sign up for My Health Record. You can then request that all your health information is updated in your online My Health Record to help you keep all your important health information together. This includes test results, medical history, pathology results, scans and X-rays and biopsies. You can access this whenever you want, and your healthcare team can too. This means that even if you have different doctors, or are seen in different locations, everyone can see your medical records.
If you choose not to have a My Health Record, get a folder and ask for a copy of all your results and healthcare communication such as letters and reports to, and from doctors and specialists. This way you can keep it altogether and share with your healthcare teams as needed.
Know your symptoms
Keep a diary of your symptoms, or add them to your My Health Record in the personal health notes section, so you can share it with your doctor without forgetting important details.
Check our Symptoms of Lymphoma webpage and share this with your doctor too. As mentioned above, many GPs may have never cared for someone with lymphoma, and no GP has cared for people with all the different subtypes, so this can be a great resource for them too.
Getting the right tests
Getting the right tests from the start is especially important when you are in RRR areas and have limited access to healthcare services. The types of tests you need will depend on your symptoms, and where in your body the lymphoma is thought to be growing. You can find more detailed information on tests for diagnosis at our webpage Lymphoma Tests, Diagnosis and Staging – Lymphoma Australia. However, as a quick guide here are some things to consider and tests that may be helpful.
Blood tests – Although we said above that many people have normal blood tests, some subtypes of lymphoma can show in your blood. In other cases, there may be signs in your blood tests that something is not quite right and needs more investigation. Blood tests can also rule out, or provide information on other possible causes of your symptoms. Helpful blood tests can include:
- Full blood count which checks your red and white blood cells and platelets.
- Electrolytes, liver and kidney function.
- Lactate dehydrogenase (LDH) which checks for damage to your cells.
- C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR) which check for inflammation.
- Beta-2 microglobulin which is a type of protein that lymphoma cells make.
Scans – If you have swollen lymph nodes your doctor can order different types of scans to check them. The scans look at the size, shape and structure of the lymph nodes. These scans may include CT-scan, MRI or ultrasound.
Biopsies – The best type of biopsy to diagnose lymphoma is an excisional biopsy. This is when the entire lymph node is removed. It allows the best chance of a diagnosis, as the pathologist can check all the cells in the lymph node and the structure of the lymph node itself.
Depending on where you are having the scans, and the part of your body where the lymphoma is thought to be growing, an excisional biopsy may not be possible at the time of your scan. In these cases, they may be able to do a core biopsy. A core biopsy takes a sample of the lymph node, or affected tissue. It is not as reliable as an excisional biopsy, but in some cases may confirm a lymphoma diagnosis.
You may need more than one biopsy to confirm a diagnosis of lymphoma.
Fine needle biopsies are NOT suitable for diagnosing lymphoma and very rarely give an accurate diagnosis for this type of cancer.
Other tests and biopsies
Other tests and biopsies may also be needed if the lymphoma is thought to be in parts of your body that are not easily biopsied. These can include a Bone Marrow Biopsy, if it is thought the lymphoma may be in your blood or bone marrow.
If the lymphoma is thought to be in your gut – stomach, bowels and oesophagus (food pipe) you may need an endoscopy or colonoscopy.
If the lymphoma is thought to be in your brain or spinal cord, you may need a lumber puncture or surgery to biopsy the area. A lumber puncture involves the doctor or nurse practitioner putting a needle in your back and into the area of fluid that surrounds your spine. They then take out a little of the fluid – called cerebral spinal fluid (CSF) to send to pathology to test for lymphoma.
Rarely, lymphoma can also start in your eyes. If this is the case, you may need a biopsy done by a specialist eye doctor. Some lymphomas can also rarely start in your brain. If this is suspected, it is likely you will need to travel to a major hospital for a biopsy to be performed by a neurosurgeon. These types of lymphoma are called Primary Central Nervous System Lymphoma (PCNSL).
Cutaneous lymphomas are lymphoma that starts in the layers of your skin. These types of lymphomas may be diagnosed with a biopsy taken through a skin scraping or other biopsy of the affected skin.
Results
Test results from biopsies can sometimes take several weeks. Always ask the person doing your tests – whether blood tests, scans or biopsies, how long results will take to get back to your doctor.
You can also choose to have your results uploaded to your My Health Record. However, you still need to make an appointment with your doctor for an explanation of the results. Some doctors will give results over telehealth or by phone, while others may prefer to see you in person. Talk to your doctor about the quickest way for you to get your results.
Don’t wait for your doctor to contact you. Be proactive in booking your appointment to make sure your results don’t get missed.
More tests
Once you get your results, you may still need to have more tests.
These tests may include tests to determine your:
- subtype of lymphoma.
- stage and activity of lymphoma – how many parts of your body are affected, and how quickly the lymphoma is growing.
- genetic features of lymphoma that help determine if you need treatment, and what treatment will likely work best for you.
You have lymphoma - What next?
Once your lymphoma is diagnosed, if you haven’t already been, you will need to be referred to a haematologist or oncologist.
- A haematologist is a specialist doctor with extra training in diagnosing, and treating people with disorders and cancer of the blood, including lymphomas.
- An oncologist is a specialist doctor with extra training in diagnosing and treating people with cancer.
Children with lymphoma are more likely to see an oncologist, while adults with lymphoma are usually treated by a haematologist. However, depending on where you live, and the specialists in your area you may be referred to either an oncologist or haematologist. Both can provide you with excellent care.
There can be delays
After getting a diagnosis of lymphoma, there can be delays in seeing the specialist doctor. These delays may be weeks or even up to 3 months. Understandably this is likely to be a stressful wait. But it’s important to understand, that with over 80 different subtypes of lymphoma, some need urgent treatment, and others don’t need to be treated at all.
Aggressive lymphomas need to be treated quickly while indolent lymphomas may not need any treatment for months or many years. About 1 in 5 people with an indolent lymphoma will never need treatment.
Is this an aggressive lymphoma or an indolent lymphoma?
How urgent is it for me to see the specialist doctor and start treatment?
Your to-do-list while waiting
It can help to have a To-Do-List while waiting for appointments. It can help take your mind of the stress of your new diagnosis (at least for a little while), while also helping you to plan for the time ahead, when you may need treatment – If you don’t have time or the energy to do these, see if a family member or friend can help.
But what do you put on your To-Do-List when you’re not sure what to expect? Below are some ideas to get you started.
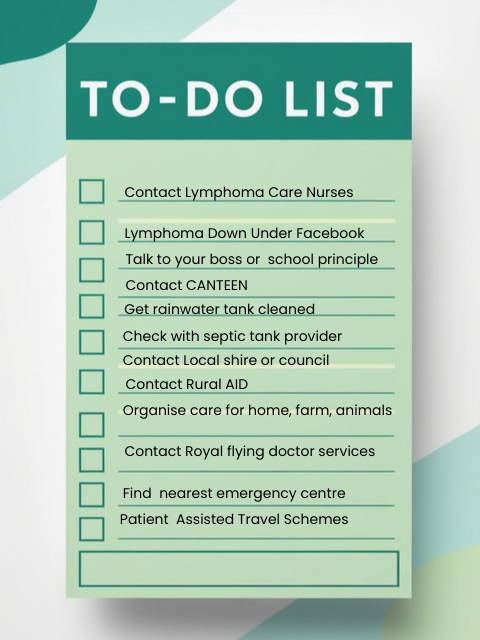
To-Do-List
- Contact the Lymphoma care nurses on 1800 953 081, or email nurse@lymphoma.org.au. They can help answer any questions you have, or refer you to who can help.
- Connect with other patients and carers by joining our Lymphoma Down Under group on Facebook, to learn about their experiences and what to expect.
- If you are working or at school and feel comfortable, talk to your boss, principle or year coordinator and let them know you may need time off, or extra support.
- If you have children, or your child has lymphoma, contact CANTEEN on 1800 226 833 and Camp Quality on 1300 662 267. They help parents and young people with cancer, and young people with a parent or sibling with cancer.
- Have your water quality checked if you use rainwater or groundwater. If you use a rainwater tank for drinking or washing in, check when it was last properly cleaned. Have it cleaned and make sure there are no broken areas for creatures to creep in. Filter and boil extra water to keep for drinking.
- If you have a septic tank, contact your service provider and check what extra precautions you may need to take, and plan ahead. We have more information on this below.
- Contact your local council or shire and ask them what support they can provide with costs of travel, accommodation and community support. Also ask about health services and organisations in nearby towns that you may be able to access if there is not one in your town when you need them.
- Contact Rural Aid on 1300 327 624. They provide a range of services including a counselling and wellbeing hotline for all people in RRR Australia. They also have a portal for primary producers, the FARM ARMY where you can post for volunteers or workers to help around the farm.
- Consider who can help look after your home, farm or animals if you need to be away for extended periods of time, during or after treatment. Also consider who can help in the event of an emergency if you need to leave quickly for medical attention. Contact them and make a plan.
- Learn about the services the Royal Flying Doctor Service can provide to you. They provide a range of services including emergency care, non-emergency transport for patients and primary health services.
- Find out where the nearest emergency centre that can cope with cancer related emergencies is. Your local council, shire or health service should be able to help you with this.
- Learn about the patient assisted travel schemes in your state.
Starting Treatment

As mentioned earlier, not everyone with lymphoma will need treatment straight away. But if you do, there are things to consider.
Firstly, there are different types of treatments you may need. These are discussed in more detail on our Treatments for Lymphoma and CLL webpage, but can include:
- Chemotherapy
- Immunotherapy
- Surgery
- Radiotherapy
- Oral therapy (tablets or capsules)
- Stem cell transplant or CAR T-cell therapy
- Clinical Trials.
The best treatment for you will depend on the subtype of lymphoma you have, the stage of your lymphoma, your age and any genetic factors found in your lymphoma. Extra considerations for you when you live in RRR Australia and are having treatment are discussed below.
Transport
As mentioned above, it is a good idea to contact your local council or shire to see if they have any programs to help with transport to and from your appointments. However, each state has transport assistance scheme as well.
Click on your state or territory below to find links to the different schemes in your area.
Western Australia
Taxi Subsidy
State transport scheme
WA Country Health Service – Patient Assisted Travel Scheme – PATS
South Australia
Taxi Subsidy
Tasmania
Taxi Subsidy
State Transport Scheme
Apply for the Patient Travel Assistance Scheme (PTAS) | Service Tasmania
Victoria
State Travel Scheme
New South Wales
Taxi Subsidy
State Transport Scheme
Isolated Patients Travel and Accommodation Assistance Scheme (IPTAAS)
Australian Capital Territory
Inter-State Transport Scheme
Queensland
Northern Territory
Transport Subsidy
State Travel Scheme
Accommodation
It is common for patients with lymphoma to have treatment in large hospitals that are usually based within, or close to city areas. Even if there is a smalller hospital nearby that offer some cancer treatments, they may not have the resources or training to provide the types of treatment you need.
In other cases, you may be able to have some treatments closer to home, but would still usually need to have at least the first treatment in a larger city hospital.
You may need treatment only on one day each cycle, or you may need treatment over several days. For this reason, it is a good idea to know what support is available to stay near the treatment centre. Below are some organisations that may be able to help with the costs of accommodation.
The National Cancer Foundation – Phone 1300 885 354.
Leukemia Foundation – Phone 1800 620 420.
MediStays – Phone 1300 085 036.
For children and young adults with lymphoma:
You Can Stay – through the Sony Foundation. Phone (02) 9383 6230.
Ronald McDonald House – Phone 1300 307 642.
Telehealth
Some appointments may be possible through telehealth. While this will not always be the case, have a chat with your doctor about what appointments can be telehealth and which ones need to be in person.
Be honest with them about the distances, costs and times it takes for you to attend in person. This will help them tailor your care to your individual needs as best they can, while maintaining a close watch on your progress.
If you have internet and phone access at home, you may be able have some appointments while remaining at home. You may also be able to access telehealth at your local doctor’s office. This can be a great option if you don’t have reliable phone/internet at home, or if you want your local GP to join the call.
Accessing Clinical Trials for Lymphoma in RRR Australia
For many people with lymphoma, clinical trials offer access to cutting-edge treatments that may not yet be widely available. However, when you live in regional, rural, and remote (RRR) areas, accessing these trials can be challenging due to distance, travel costs, and limited trial locations.
Most clinical trials are based in major cities, requiring you to travel for assessments, treatments, and follow-ups. This can be physically and financially exhausting, especially when juggling work, family, or farm responsibilities. However, being in a rural area doesn’t mean missing out—self-advocacy and knowing where to look for trials can make all the difference.
How to Advocate for Yourself
- Ask your doctor: Some local oncologists or haematologists have connections with trial coordinators and may help you access trials closer to home.
- Request telehealth options: Many trials now offer remote consultations, reducing the need for travel.
- Check if local hospitals participate: Some regional centers collaborate with city-based trials to provide treatment closer to home.
Where to Find Clinical Trials
- Australian New Zealand Clinical Trials Registry (ANZCTR) – www.anzctr.org.au
- ClinTrial Refer App – Lists available trials in Australia by location and condition. Check your apple or android app store.
- Lymphoma Australia Nurses – Can offer support and guidance on trial options. Call 1800 953 081, Monday – Friday 9am – 4:30pm AEST (Sydney time).
Making Trials More Accessible
Some trials allow treatments to be administered locally while major assessments happen in larger centers. Speak to the trial coordinators about flexible options. If travel is required, ask them about financial support programs that help cover transport and accommodation costs.
By staying informed and advocating for options, you can increase your chances of accessing life-changing treatments without completely uprooting your life.
Am I eligible for any clinical trials?
Can I access these closer to home?
Are these available through telehealth?
Do any local hospitals participate in clinical trials for lymphoma?
Side-effects - Extra consideration in RRR Australia
Cancer treatment comes with side effects that can impact your daily life, making tasks like driving, working on the farm, or operating machinery and small planes riskier. It’s important to recognise these challenges and take steps to stay safe.
Fatigue & Weakness
Cancer treatments, especially chemotherapy and radiation, can leave you feeling exhausted. Fatigue can make simple tasks harder and increase the risk of accidents, especially when driving long distances, working with heavy equipment or operating machinery or aircraft. Where possible, make a plan to take time off work, decrease your hours or have someone else do the heavier tasks until you recover.
Plan for regular rest breaks, avoid driving when tired, and ask for help when needed.
Pain & Nerve Damage
Nerve pain (neuropathy) and muscle weakness are common after treatment, affecting your grip, balance and coordination. This can be dangerous when handling machinery, climbing ladders, or even walking on uneven ground.
Wear supportive footwear, use handrails, and take extra precautions with tools and vehicles.
Chemo Brain & Concentration Issues
Many patients experience chemo brain or brain fog, which can include trouble with memory, focus, and decision-making. This can make tasks like operating farm equipment, flying small planes, or managing finances more difficult.
Keep lists, set reminders, and avoid high-risk activities if you feel foggy or distracted.
Anxiety & Emotional Wellbeing
We understand that farmers and those in regional, rural, and remote areas are resilient and tough, yet also face significant challenges—even before the added stress of a lymphoma diagnosis. The impact of treatment, isolation, and financial strain from time off work and healthcare costs can take a toll on mental and physical well-being. This may impact your sleep, focus, and reaction times. Staying connected with support networks and reaching out for professional help when needed can make a real difference.
Recognising these risks, having a plan and adapting daily tasks can help you stay safe while continuing to enjoy life in the bush. Below are some important numbers and links to organisations that can help you in a crisis, or to make a wellbeing plan.
- Lymphoma Nurses on 1800 953 081 Monday-Friday, Monday – Friday 9am – 4:30pm AEST (Sydney time).
- Rural Aid to talk to an experienced counsellor who is based in a rural town. Phone 1300 175 594.
- Lifeline for general counselling and suicide prevention. Phone 13 11 14.
- Beyond Blue for general counselling and creating a wellbeing plan. Phone 1300 22 4636.
Financial Support
A lymphoma diagnosis and its treatment can create financial strain; Especially if you are unable to work for long periods of time. While some people are able to continue work as normal, some need lighter duties, decreased hours or time off completely.
Receiving financial support can be complex, but there are some financial support payments available through various government organisations such as Centrelink, Medicare and Child Payments. Your spouse or someone close to you helping to care for you while you are unwell may also be eligible for carers payments or allowances.
You may also be able to access some payments through your superannuation fund.
If you have a financial advisor, let them know about your lymphoma so they can help you plan how to manage your money. If you do not have a financial advisor, you can access one through Centrelink. Details on how to access a Centrelink financial advisor are below under the heading Centrelink.
Click on the buttons below to learn about what support is available.
Medicare
Medicare can help cover medical costs and advise on how to keep costs down. Information on the various Medicare payments and services available can be found here.
Child payments
- Carer adjustment Payment is a one-off payment. It helps families when a child younger than 6 is diagnosed with one of the following:
- a severe illness
- medical condition
- major disability
- Child Disability Assistance Payment is a yearly payment to help parents with the costs of caring for a child with disability.
- Essential Medical Equipment Payment is a yearly payment to help with increases to home energy costs. This can be from the use of essential medical equipment to help manage disability or a medical condition.
Superannuation
While superannuation is usually protected until you turn 65 years of age, in some circumstances you may be able to access some of it on ‘compassionate grounds”. Some situations that may be considered compassionate grounds include:
- Paying for medical treatment (or transport to and from treatment).
- To help with your mortgage if the bank is about to foreclose (take possession of your house).
- Renovations if you need to modify your house due to injury or illness.
- Pay for palliative care.
- Pay expenses related to the death of one of your dependants – such as funeral or burial costs.
You can get more information on accessing your superannuation on compassionate grounds, by phoning the Federal Department of Human Services on 1300 131 060.
Insurances built into superannuation
Many superannuation funds have a built in ‘income protection’ or total permanent disability payment in the policy. You may have this without even knowing it.
- Income protection covers a portion of your normal wage/salary when you are unable to work due to sickness or injury.
- Total permanent disability is a lump sum paid out to you if you are not expected to get back to work due to your illness.
Your insurances will depend on your superannuation company and policy. If you are unable to work due to your lymphoma, contact your superannuation fund and ask what support and insurances are built into your policy.
Extra help with Superannuation and finances
If you are having trouble accessing your superannuation or insurance policies, Cancer Council Australia has a pro bono program that may be able to help with legal advice or other support to help you access these. You can find more information about the support they can provide by clicking here.
If you still have no luck, you can make a complaint with the Australian Financial Complaints Authority. Other useful links can be found here.
Centrelink
People with disability, illness or injury, and their carers can call Centrelink on 13 27 17 to enquire about payments and services available. Click on the following link to read: A Guide To Australian Government Payments.
Some of the Centrelink payment services include:
- Sickness allowance: An income support payment if someone is unable to work or study for a period of time due to illness, injury or disability.
- Carer allowance: additional payment (bonus) subsidies the carer payment (in-additional) can earn up to 250,000/year (roughly $131/fortnight) can work 25 hours and still be on this.
- Carer payment: An income support payment if you give constant care to someone who has a severe disability, illness or is frail aged.
- Click the following link to learn more about Carer Payments.
- Click the following link to read How to Claim Carer Payments.
- Disability support pension: Financial support for permanent intellectual, physical or psychiatric disability that stops patients from working.
- Download and complete the ‘Claim for Disability Support Pension’ form
- Disability benefits: There are payments and services to help if you are ill, injured or have a disability.
- Payments for Children
- Mobility allowance: You may be able to access mobility allowance if you have lymphoma and are unable to use public transpont. This can be used need to travel for study, training work (including volunteering) or to look for work. See more by clicking here.
- Job Seeker allowance: If you are on Job Seeker allowance and are unable to look for work due to your lymphoma or its treatments, ask your doctor – GP or heamatologist to fill our a Centrelink Medical Certificate – form SU415. You can get to the form by clicking here.
Social Workers
If you need help to understand or access centrelink services, you can ask to speak to one of their social workers who can help you work out what you may be entitled to, and how to access it. You can contact a Centrelink Social Worker by phoning 13 27 17. Ask to speak to a social worker when they answer and they will put you through. You can also look at their website here Social work services – Services Australia.
Financial Information service
Another service Centrelink provides is a Financial Information service to help you plan how to make the most of your money. Phone them on 13 23 00 or see their webpage here Financial Information Service – Services Australia
You can find extra information on payments and support through Services Australia at their Community Resources and Help page here.
Bills, Food & Other Financial Support
Some organisations can help with paying bills, food parcels, and other finances. Below are list of organisations that may be able to help you.
The Salvation Army – Phone: 13 72 58.
St Vincent De Paul Society – Phone: 13 18 12.
Can Assist – For RRR patients in NSW only. Phone: 1300 226 277.
Rural Aid – For Primary Producers in RRR Australia. Phone: 1300 327 624
Also check with your local council or shire, churches, Country Woman’s Association (CWA) and community organisations that may be able to offer some support. Many will not only provide financial support, but may be able to help with practical things like meals, cleaning, gardening and transport too.
Bodily waste and septic tank systems
Some treatments for lymphoma are excreted in your bodily waste, such as your urine (wee), faeces (poo), blood and other bodily fluids. Because of the toxic nature of these treatments, they can interfere with the bacteria needed to keep your septic tank system working properly by:
Killing the good bacteria – Your septic system needs good bacteria to help break down the waste. Some treatments for lymphoma that are excreted through urine and faeces can kill or damage these good bacteria. When this happens you could have buildup of solid waste in your septic system, resulting in a buildup of bad bacteria, and clogging your system.
Impact on leach field – If your septic system is not working effectively, it can have an impact on the leach field with residual chemicals and bacteria seeping into the soil. This can result in contamination of the surrounding environment.
Contact your Septic Tank System Maintenance Company
Talk to your septic tank specialists about how you can reduce the harm and maintain a healthy functioning septic system. They will be able to give you the best advice on how to manage the system during and after treatment. However, some things to consider may include:
- Adding good bacteria to the system which may help maintain the levels needed to keep your system working properly. These can be bought at many local hardware stores or through your septic tank maintenance provider. Use these as directed because even too high levels of good bacteria can result in harm to your septic system.
- Have your system pumped more frequently. How often will depend on the type and length of your treatment. Ask your maintenance provider about how often this should happen.
- If you don’t already have an aerobic remediation system, it may be worth considering having one installed. These can increase biological activity in the septic system to help with the breakdown of waste.
- Maintain proper use of the septic system and ensure everyone using the system avoids putting harsh chemicals, grease, non-biodegradable waste, such as tampons or overly thick toilet paper down the system.
Rainwater tanks, Groundwater and Lymphoma
Having lymphoma can lower your immune system due to it being a cancer of lymphocytes – white blood cells responsible for fighting disease and killing germs. When you add to that, treatments for lymphoma that can kill off even more of your immune cells, managing your risks for infection becomes very important.
Many people in RRR areas of Australian rely on water collected from underground (bore water) or in rainwater tanks. When you have a functioning immune system, the risk of infection from these water sources is low, and even if you get an infection, you can usually fight it off without too much trouble.
But when your immune system is compromised from your lymphoma and – or its treatments, even minor infections can cause great concern and risk to your health. Some infections can become life-threatening quickly.
With this in mind, it is important to consider the quality of water that you drink and wash in.
What can affect water quality in RRR Australia
Many things can contaminate your water sources. These can include run off contaminated by animal faeces, dead animals, chemicals including pesticides and herbicides, plastics and rubbish, sewage, as well as contaminates from natural disasters such as flooding and bushfires.
While some things maybe within your control, such as keeping overlying branches away from water sources and ensuring an environment free of rubbish, chemicals and animal carcasses or waste; Not everything can be controlled. Have your water quality checked before you start, and as you go through treatment. You can also filter and boil water to remove contaminants. Take care to let water cool in a safe place before using or drinking it.
For more information on maintaining safe water quality see the links below.
Staying Safe
Infection and Bleeding Risks for People with Lymphoma in RRR Australia
While living in the bush, on a farm or in a small country has it’s perks, keeping safe while living with lymphoma adds extra challenges. Having a lowered immune system, and treatments that can increase your risk of infection and bleeding are unfortunately the reality. And, when your far away from emergency services, or even local doctors there are extra considerations you need to be aware of.
Creepy Crawlies and Bites
Snakes, spiders, mosquitoes, and ticks are part of life in the bush, but if your immune system is weak, a bite or sting can lead to infection or a more severe reaction than usual.
- Snakes: If bitten, stay still to slow the venom’s spread, apply a pressure bandage, and get help immediately. Always wear boots and long pants when walking in long grass or bushland.
- Spiders: Some bites can cause tissue damage or serious infections, especially if your body struggles to fight bacteria. Check shoes, gloves, and bedding before use.
- Mosquitoes and Ticks: These can carry diseases that your body might struggle to fight off. Use insect repellent, wear long sleeves, and check your body for ticks after being outdoors.
Farming and Machinery Accidents
Many people in regional and remote areas work on farms, handle animals, or use heavy machinery. These jobs come with a high risk of cuts, bruises, and crush injuries. Talk to your doctor about what type of work or home maintenance you do and if it is safe to continue doing these. You may need to take time off and get someone else to do these things for you. However, where it is unavoidable, you still need to know what to do if something goes wrong.
If your blood doesn’t clot properly, or your immune system is compromised due to cancer or treatment, even a small cut can become a big problem.
- Always wear gloves, long sleeves, and protective gear.
- Keep a well-stocked first aid kit with antiseptic wipes, bandages, and clotting powder.
- If you cut yourself, clean the wound immediately and apply firm pressure. If the bleeding is severe, or doesn’t stop within 10 minutes, seek help.
- Be extra cautious with power tools and machinery—any injury could lead to uncontrolled bleeding or infection.
- Notify your doctor or community nurse, or contact the Royal Flying Doctor service and seek advice.
Infections from Dirt, Animals, and Water
Cancer treatment can lower your white blood cell count, making it harder for your body to fight infections. Farm work, gardening, and handling animals exposes you to bacteria, fungi, and parasites that can cause serious illness.
- Wear gloves when gardening or handling soil, as bacteria like Clostridium (which causes tetanus) and fungi can enter through small cuts.
- Wash scratches and bites from animals immediately with soap and water, and apply antiseptic. Even a small wound can become infected quickly when you have lymphoma.
- Avoid cleaning animal waste or stagnant water to reduce exposure to harmful bacteria and parasites. Ask someone else to do these for you. If it is unavoidable, make sure any wounds are covered, wear long sleeves, a mask and gloves. When finished remove gloves first, wash your hands, then remove other protective gear and wash your hands again.
- Stay up to date with vaccinations like tetanus and flu shots to reduce infection risk.
Update first-aid and CPR certificates
Knowing you have lymphoma and may be starting treatment is a great opportunity to encourage everyone in your household, workplace or even community to update, or complete a first-aid course.
Rural and Remote First Aid offers courses with special attention to the extra challenges faced by RRR Australians. You can contact them at their website or by phoning 0491 057 339.
You can also contact your local council, shire, or community hub to find out if there are any community first-aid courses running near you.

Essential First-Aid Kit for Lymphoma Patients in RRR Australia
Living far from major hospitals means you need to be prepared for medical issues that may arise due to a weakened immune system, increased bleeding risk, and dehydration. Here’s a list of essential first-aid items every cancer patient should have at home, and in a portable first-aid kit.
Bleeding Control & Bruising
- Blood clotting powder (e.g., HemCon, Celox, or similar) – Can slow heavy bleeding but should only be used under medical guidance.
- Compression bandages – To control bleeding from larger wounds.
- Cold packs (instant or freezer) – To reduce swelling and bruising.
Managing Dehydration & Electrolyte Imbalance
- Oral rehydration salts (e.g., Hydralyte, Gastrolyte) – To prevent dehydration.
- Electrolyte drinks or powders – Helps maintain hydration levels, especially during vomiting or diarrhea, or if stuck or working on a hot day in the middle of nowhere.
- Thermometer – To monitor for fever, which can signal infection or heat exhaustion.
Pain Relief & Fever Management
- Paracetamol (Panadol, Tylenol) – Safe for fever and mild pain but should be used cautiously.
- Topical pain relief (e.g., Lidocaine gel, Deep Heat, instant heat and cold packs) – For muscle aches and joint pain.
- Anti-nausea medication (as prescribed by your doctor) – For managing chemotherapy side effects.
Allergy & Bite Protection
- Antihistamines (e.g., Telfast, Claratyne, Zyrtec) – For allergic reactions or insect bites.
- Hydrocortisone cream – To reduce itching and inflammation from bites or rashes.
- Insect repellent (DEET or Picaridin-based) – To prevent mosquito and tick bites.
Infection Prevention & Wound Care
- Sterile gloves – For safe wound care and infection control.
- Antiseptic wipes/spray/cream (e.g., Betadine, Chlorhexidine, Tea tree oil, Rubbing alcohol, Savlon) – To clean cuts and prevent infection.
- Sterile gauze pads & dressings – To cover wounds and keep them clean.
- Adhesive bandages (plasters in different sizes) – For small cuts and abrasions.
- Medical tape – To secure dressings without irritating the skin.
- Antibiotic ointment (e.g., Bactroban or Neosporin) – To prevent wound infections.
- Tweezer & splinter remover – For removing foreign objects safely.
- Hand sanitiser
Emergency Medications & Supplies
- Broad-spectrum antibiotics (if prescribed) – Ask your doctor if an emergency supply is appropriate, especially if you live far from medical services.
- Epinephrine auto-injector (if at risk of anaphylaxis) – For severe allergic reactions.
- Blood pressure monitor – To check for sudden drops or spikes.
- Medical alert bracelet – So emergency responders can see you have lymphoma, and any other serious conditions.
Important Notes on Antibiotics and Blood Clotting Powder
If you live in a remote area, discuss with your doctor whether having a backup supply of broad-spectrum antibiotics (such as amoxicillin/clavulanate or cephalexin) is appropriate for emergency infections. However, never self-medicate without medical advice, as improper use can lead to antibiotic resistance.
Blood clotting powders can be lifesaving for those at high risk of bleeding, but they should only be used under a doctor’s guidance. Inappropriate use can cause complications, so learn when and how to use them correctly.
Regularly check expiry dates on all medications and first-aid supplies, and store everything in a clean, dry, and sterile environment. Having a well-prepared kit can be the difference between a minor issue and a medical emergency when living far from help.
When Help is Far Away
Getting to a hospital quickly isn’t always possible in the bush, so having a plan is essential.
- Know your closest emergency services and how to reach them.
- Talk to your doctor about an emergency plan, including when to go to the hospital.
- Keep emergency contacts handy, including the Royal Flying Doctor Service if you’re in a remote area.
- Consider a medical alert system or personal emergency beacon if you live alone or travel often.
- Have extra medical supplies on hand, including antibiotics (if prescribed) and clotting agents.
Summary
Challenges Faced by RRR Lymphoma Patients:
Limited Access to Specialised Care: The lack of oncology & haematology specialists in RRR areas means you may need to travel to large city centers for treatment, which can be a financial, time consuming and emotional burden.
Financial Strain: Travel expenses, accommodation costs, and time away from work can lead to significant financial hardship. This page has provided information on financial support you may be able to access for general bills, travel, accommodation, and other support through organisations such as Centrelink, your superannuation fund and community organisations.
Psychosocial Impact: Isolation from support networks and the stress of managing a serious illness with limited resources can adversely affect mental health. It is common for people with lymphoma, and their loved ones to experience changes in mood and emotions. Living away from home for treatments, or fear of being away from health services adds extra challenges when you are in RRR Australia. This page has provided links and contacts for different support groups and services you can access, including those with unique understanding of RRR challenges.
Time Commitment: When you live far from primary health or treating centres you may need to consider time away from home. Some treatments for lymphoma, side effects and illness may result in you needing to be admitted to hospital, or stay close to your treating center. This may be for a few nights or even months. We have provided some practical tips above on how to manage this.
- Distance to health services when things go wrong: If you become unwell or have an accident there are always concerns about being far away from medical help. However, when you have lymphoma and treatment, your immune system, or blood clotting may be affected resulting in further problems. We have provided tips on keeping yourself safe, and how to get urgent help if needed.
Support Strategies and Resources:
Telehealth Services: Advancements in telemedicine enable patients to consult with healthcare providers remotely, reducing the need for travel and facilitating timely medical advice.
Local Healthcare Collaboration: Engaging with local general practitioners and rural cancer nurses can enhance care coordination, ensuring that treatment plans are effectively implemented close to home.
Financial Assistance Programs: There are organisations that offer support to help with the financial burdens of treatment, including assistance with travel and accommodation.
Accessing Clinical Trials: This can be challenging for RRR patients due to distance. However we are encourage you to discuss potential opportunities with your doctor. Some trials may offer remote participation and use telehealth options, or they may collaborate with local healthcare providers to facilitate involvement.
Community and Online Support: Connecting with support groups, either locally or through online platforms, can provide you with emotional support and practical advice, helping to overcome feelings of isolation.
Royal Flying Doctor Service: The Royal Flying Doctor Service provides both primary and emergency care. If you live far from healthcare centers, explore their website or give them a call to see how, and when they can help you.
Contact Lymphoma Care Nurses: Lymphoma Australia has highly experienced lymphoma nurses who can help provide information and resources. You can contact them Monday – Friday 9am – 4:30pm AEST (Sydney time), on 1800 953 081 or email them on nurse@lymphoma.org.au
Final thought
There are extra challenges when diagnosed with lymphoma and living in RRR Australia. However, with some forward planning, understanding the support available to you, and having the confidence to advocate for yourself, you can still enjoy the country life while getting the best possible care.