What does aggressive mean?
Aggressive refers to how your lymphoma cells behave and grow. They are fast-growing, and no longer behave in the organised way expected of healthy cells. As a result, they can no longer work properly to protect you from infection and disease.
The pathologist can see how your cells grow and behave by looking at them under a microscope. But you may also be able to tell that the lymphoma is aggressive, because the signs and symptoms of aggressive lymphoma happen over a very short time-frame. For example, you may notice a lump comes up in your neck, armpit or groin very quickly – this can mean in a day, or over a couple of weeks or months, and does not improve. These lumps are a result of your lymph nodes filling up with cancerous lymphoma cells.
However, there are other reasons your lymph nodes can swell such as infection or allergies. These lumps usually go down on their own, or after antibiotics and within 2-3 weeks. With lymphoma, they will continue grow or remain swollen.
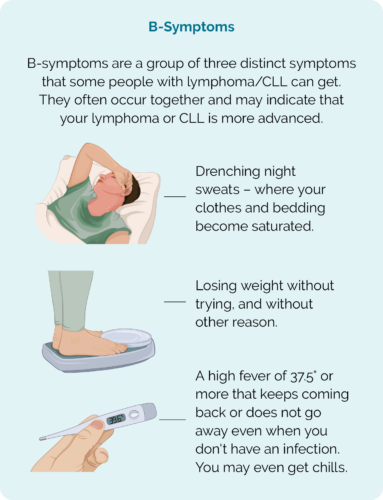
You may also get B-symptoms.
Are aggressive lymphomas curable?
Many aggressive B-cell lymphomas respond very well to treatment. This is because some anti-cancer treatments, such as chemotherapy work by destroying fast-growing cells – making them particularly affective against aggressive lymphoma. This means, many people with aggressive B-cell lymphomas can be cured or have long periods of time in remission.
What's the difference between a cure and remission?
Unfortunately, not all aggressive lymphomas are equal so the way they respond to treatment can vary between people. There are many factors that can impact how your lymphoma will respond and your specialist haematologist or oncologist will discuss these with you.
The aim of treatment can be different depending on your individual circumstance. Things that can impact the aim of treatment include the subtype of lymphoma you have, genetic mutations within your lymphoma cells, your overall health and other things. It is really important to understand why you are having treatment and what to expect.
Ask your doctor what the aim of your treatment is and if you should expect to be cured or go into remission. To understand the difference between cure and remission, click on the boxes below.
Cure
Complete remission
Partial remission
What happens when aggressive lymphoma relapses or does not respond to treatment?
In some cases, your lymphoma may be refractory to treatment – meaning it does not respond and get better with the treatment you are given. In other cases, it may respond well to the treatment, and you may go into remission, but the lymphoma comes back – relapses.
Whether your lymphoma is refractory or relapses, you will most likely need to have more tests and start a different type of treatment. The next treatment will be considered a second-line treatment and may be similar to what you’ve had previously or very different.
Many people still have a good response to second-line treatments and can still achieve cure or remission. To learn more about relapsed and refractory lymphoma, click the link below.
What subtypes of lymphoma are aggressive?
There are more than 80 different subtypes of lymphoma. The more common aggressive B-cell lymphomas are listed below. To read more, click on the one you are interested in.
Summary
- Aggressive lymphomas are lymphomas that start and grow quickly. You may notice signs and symptoms start over a period of days or a months. These can include a swollen lymph node that does not go down or B-symptoms.
- Many aggressive lymphomas respond well to treatments as the treatment is designed to destroy fast-growing cells.
- Many aggressive lymphomas can be cured or have long times of remission.
- If your aggressive lymphoma does not respond to treatment (is refractory) or relapses you will likely need second-line treatment which can still be effective.
- Talk to your specialist oncologist or haematologist about what to expect from your treatment.
- If you would like to speak with a lymphoma care nurse, click on the “Contact Us” button at the bottom of the screen.

