Overview of Peripheral T-cell Lymphoma – Not Otherwise Specified (PTCL-NOS)
Although PTCL-NOS is the most common subtype of PTCL, it is a very rare cancer. It starts when T-cell lymphocytes – a type of white blood cell undergo changes that causes them to become cancerous. These changes happen in your genes which make up your DNA. Every cell that makes up every part of our body, except our red blood cells has a nucleus that contains all our DNA.
We don’t know why these changes happen in some people and not others.
Who is affected by PTCL-NOS?
Around 1 in 3 people with PTCL will have PTCL-NOS. It is more common in people aged over 60 years, but people of any age, including children can develop it.
Symptoms of peripheral T-cell lymphoma – NOS (PTCL-NOS).
PTCL-NOS can be nodal or extra-nodal.
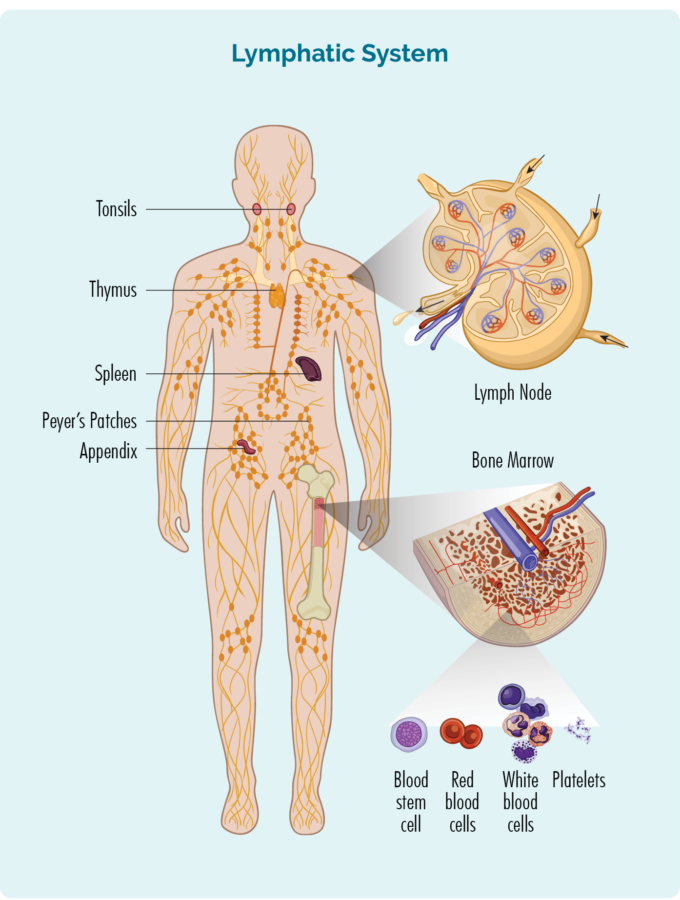
Nodal means it starts when the lymphocytes in your lymph nodes become cancerous. We have lymph nodes all through our body, and it can start in any of the lymph nodes. You can see the lymph nodes in the picture as the little yellow oval spots found mostly in the neck, armpits, chest, and abdomen, but there are also more in the arms, legs and head.
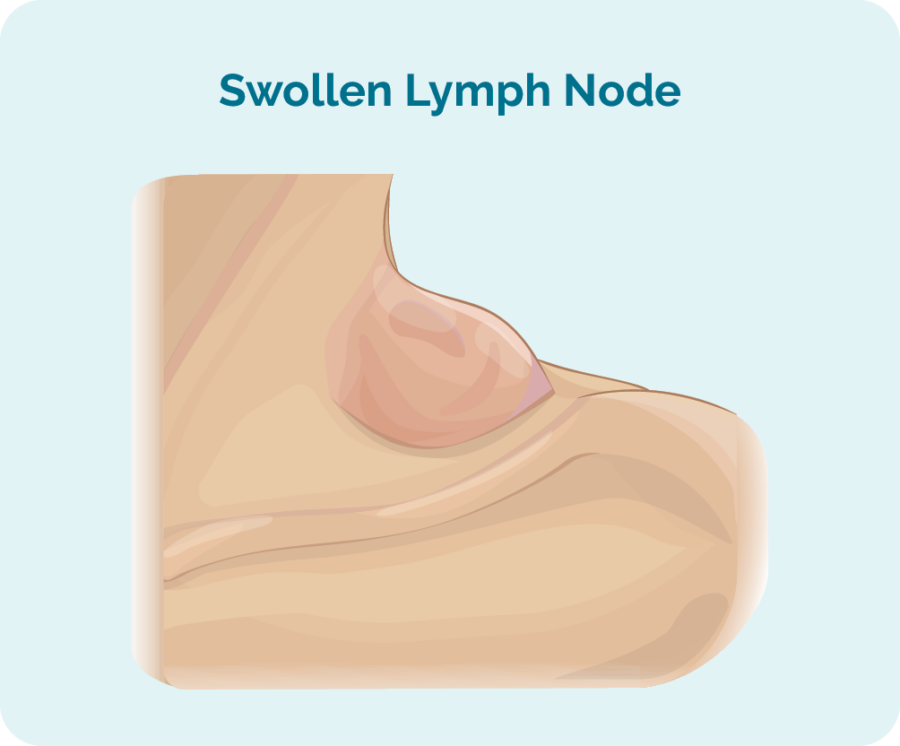
The most common, and often first symptom of nodal lymphoma is when lymph nodes becomes swollen and appears like a lump under your skin that you can see or feel.
Extra-nodal means the lymphoma starts outside of your lymph nodes. This can be in your organs, bones, bone marrow or even in your skin. Symptoms of extra nodal lymphoma are often different to nodal because you may not have any swollen lymph nodes.
Instead your symptoms are more likely to be related to the area the lymphoma is growing. For example, if it is growing in the layers of your skin, you may have a rash or lumps in your skin. If it is growing in your bone marrow, you may have changes in your blood tests.
Other commons symptoms of PTCL-NOS
Common symptoms may include:
- Swollen lymph nodes-most commonly seen or felt in the neck, armpit, or groin.
- Anaemia (low red blood cells) and thrombocytopenia (low platelets) if you have lymphoma in your bone marrow.
- Bloating and abdominal pain because your spleen and liver can become bigger than they should be.
- Loss of appetite, not wanting to eat.
- Itchy red patches or rashes on your skin.
- Chest pain or shortness of breath.
- Fatigue extreme tiredness not improved with rest or sleep.
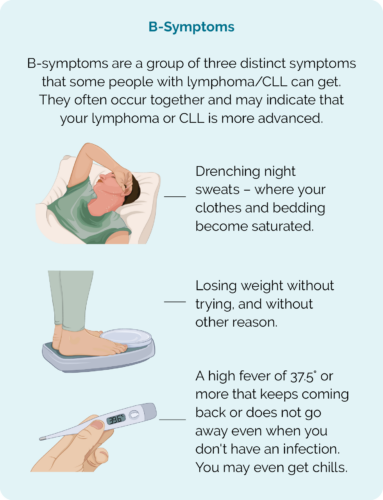
B-symptoms
B-symptoms are specific symptoms that may indicate your lymphoma is growing quickly and that you may need to have treatment soon. However, you may still need urgent treatment even if you don’t have B-symptoms.
Report all new or worsening symptoms to your doctor. If you have reported them before and they have not improved, let your doctor know so they can assess you properly and make the right plan for you.
Diagnosis and Staging of PTCL-NOS
To diagnose lymphoma you will need a biopsy of your swollen lymph nodes or other affected tissue – such as a skin biopsy or bone-marrow biopsy. A biopsy is when they take a sample of the affected area to look at and test in pathology.
This may be done with the doctor using a needle with a local anaesthetic to numb the area, or in surgery under a general anaesthetic depending on the area being biopsied.
Staging
Is when you have extra tests to see how much of your body is affected by the lymphoma , or how far it has spread.
To learn more about diagnosis and staging click on the link below.
How is PTCL-NOS treated?
The type of treatment you get for PTCL-NOS will depend on several things. These can include:
- Your age and overall physical and mental health.
- If you have ever had treatment for the same or different lymphoma in the past.
- What other conditions or illnesses you may be having treatment for.
- The stage of your lymphoma and symptoms you are getting.
- Whether your lymphoma is nodal or extra-nodal.
- What parts of your body are affected.
- Results of the genetic tests on the lymphoma biopsies.
- Your own preferences after you have been given a chance to discuss all your options and concerns with your doctor.
Treatment will be based on your individual circumstances. The first time you have treatment it is called first-line treatment. First-line treatment usually lasts for several cycles. Your doctor will be able to let you know how many cycles of treatment you will have in your first line treatment.
Before you start treatment
Before you start treatment there are some things you need to consider and prepare for.
Fertility
Many treatments can affect your fertility, making it more difficult or impossible to get pregnant, or get somebody else pregnant. If you are of child-bearing age, even if you are not thinking about having a family or extending your family just yet, you need to talk to your doctor about how to preserve your fertility, or prevent unwanted pregnancies. For more information on fertility, click the link below.
Questions to ask your doctor
When you are first diagnosed, or starting treatment after a relapse, it can be difficult to think straight and know what questions to ask. It is important you have all the right information you need to make the decisions about your healthcare and to know what to expect. Click on the link below to download Questions to ask your doctor.
Practical things you need to know and how to prepare
Having treatment is going to change your life and the lives of those closest to you for a while. It is important to know what to expect and prepare for. You also need to know what support is available to you. We have developed some tips on practical things you should know when you or a loved one has lymphoma. Click the link below for more information.
First & Second-line treatments
First-line treatment can be very effective at putting lymphoma in remission, or in some cases even curing the lymphoma altogether. However, in some cases, PTCL-NOS may relapse, which means it comes back and will need more treatment. When you have treatment a second time it is called second-line treatment.
You may also need second-line treatment if your lymphoma is refractory to the first-line treatment, which means it doesn’t improve with the first-line treatment. For more information on relapsed and refractory lymphoma click further down the page after treatments.
Radiotherapy uses high-energy x-rays (radiation), to kill cancer cells. It can be used as a treatment on its own, or with other treatments such as chemotherapy. Sometimes it can be given after you have had surgery, to make sure there are no lymphoma cells left.
There are different reasons your doctor may suggest radiation treatment for you. It can be used to treat and possibly cure early PTCL-NOS, or it can be used to improve symptoms. Some symptoms such as pain or weakness may happen if your lymphoma tumour becomes too large, or is putting pressure on your nerves or spinal cord. In this case, the radiation is given to shrink the tumour and relieve the pressure. However, it is not intended to be used as a cure.
If you only have lymphoma in one area of your body and it can be safely removed completely, you may only need to have surgery with a high chance of curing your lymphoma. In some cases, you may be offered radiation treatment to have after surgery to be sure there are no lymphoma cells left.
Chemotherapy are medicines that work by destroying fast-growing cells, so they can be very effective at treating aggressive – or fast-growing lymphomas like PTCL-NOS. However, chemotherapy cannot tell the difference between fast growing cancer cells and fast-growing healthy cells.
For this reason, chemotherapy is given as a combination of medicines in cycles. This means you will often have more than one type of chemotherapy to limit the side-effect of each one. It will also be given as cycles, so you will have the chemotherapy then a break of up to 3 weeks and then more chemotherapy. How many cycles you have will depend on your individaul circumstances and chemotherapy protocol.
Monoclonal antibody
If your lymphoma cells have a specific protein called CD30 on them, your doctor may also recommend including monoclonal antibody called brentuximab vedotin to your treatment protocol. This medicine is only effective if you have the CD30 protein.
First-line treatment
First-line treatment refers to the first lot of treatment you have. This usually includes several different types of chemotherapy. The treatment protocol your haematologist or oncologist recommend to you will depend on your individual circumstances including your overall health and any genetic factors found in your biopsies. Some common protocols are listed below, but you may be offered something different to these.
CHOP – cyclophosphamide, doxorubicin, vincristine and a steroid called prednisolone
CHOEP – same as CHOP but with an extra chemotherapy called etoposide.
Second-line treatments
Second-line treatments may include the above if you have been in remission for a long time. however, you doctor may recommend different types of chemotherapy that may work better for you. These can include:
Gemcitabine and vinorelbine.
Pralatrexate.
Romidepsin.
DHAC – Steroid called dexamethasone, and chemotherapies cytarabine and carboplatin.
DHAP – steroid called dexamethasone, and chemotherapies cytarabine and cisplatin.
ESHAP – cisplatin, etoposide, cytarabine, and a steroid called methylprednisolone. You will also have an injection called pegfilgrastim to help your white blood cells recover.
GDP – gemcitabine, dexamethasone (steroid) and cisplatin.
ICE – ifosfamide, carboplatin and etoposide.
Depending on your age and overall health, you may be offered a stem-cell transplant as part of your second-line treatment. Stem cells are a rescue treatment given to replace your blood cells after being given high doses of chemotherapy. Because high-dose chemotherapy destroys all your blood cells you need to be relatively fit and young (less than 65 years) to cope with the chemotherapy side-effects.
A stem-cell transplant is a rescue treatment to save you from the effects of high dose chemotherapy. The high-dose chemotherapy is the treatment for your lymphoma, and the stem-cells replace the blood cells killed off by the high dose chemotherapy.
By having a stem-cell transplant after chemotherapy, you can be given much higher doses of chemotherapy that you would normally not survive if not for the stem cells transplant.
Depending on your age and fitness, you may be offered a stem cell transplant at the end of first-line treatment. Many hospitals also have an age cut off of about 65 years because as we age our bodies are less able to cope with the stress our bodies would be under with the high-dose chemotherapy.
If you did not have a stem-cell transplant after your first-line treatment and your lymphoma relapses, you may still be offered a stem-cell transplant as a second line treatment.
More information on stem-cell transplants can be found here.
Clinical trials are how researchers are able to find new treatments to improve outcomes for people with lymphoma. They can include new medicines, combinations or doses of medicines or different types of treatment altogether.
PTCL-NOS is a rare cancer, and so clinical trials offer a way to find what treatments work best for you. However, there are no guarantees with clinical trials, as their purpose is to find out if the new treatment can work better than current treatments. In some cases they may work better, and others may not be as effective. There is no way of knowing if you will get a better response in a trial or with current treatments.
That said, we always recommend you ask your doctor about what clinical trials you may be eligible for and what the benefits and risks of the trial are. Clinical trials may be offered at any point along your treatment pathway.
Then you can make a decision based on your lymphoma and the trial information given. More information on clinical trials can be found here.
Side effects of treatment
Everybody responds to treatments differently, and the types of side-effects you get will depend on the treatments you are having, your overall health, where in your body your lymphoma is among other things.
Some side-effects are more common that others. To learn more about side-effects oc treatments, how to manage them home and when to see your doctor, click the link below.
Finishing treatment

Finishing treatment can fill you with all sorts of emotions. You may be excited that treatment is over and you can start to think about life again, or you might be worried about not seeing your doctors and nurses as often as you used.
Whatever you are feeling, you are entitled to feel it. There is no right or wrong way to feel about finishing treatment, and it’s important to know that even when treatment stops, you will not be left on your own. Nor will life get straight back to normal.
Follow up appointments
You will still have regular appointments with your haematologist or oncologist. They will do a physical examination of your lymph nodes and check blood tests results and ask you about any symptoms or ongoing side-effects you may have. You may even have follow-up PET or CT scans, though this will depend on your individual circumstances.
Late or ongoing side-effects
In most cases, your side-effects from treatment will improve within weeks or months of finishing treatment. However, rarely, you can have side-effects that need long term management, or that start long after treatment finishes.
Report all ongoing or new symptoms and side-effects to your doctor so they can assess and advise you properly on how to manage them.
Summary
- PTCL-NOS is a very rare type of cancer but is the most common subtype of Peripheral T-cell Non-Hodgkin Lymphomas.
- It can be nodal or extra-nodal and your symptoms will depend on where your lymphoma is growing.
- You may have B-symptoms if it is growing quickly, but not always.
- PTCL-NOS is usually an aggressive type of lymphoma that needs treatment very soon after you are diagnosed.
- There are several different types of treatment you may be offered, and the best one for you will depend on your individual factors.
- Knowing what side-effects you may get and how to manage them and when to contact your doctor can help stop them getting too bad.
- PTCL-NOS often responds well to first-line treatment, but can relapse and need more treatment.
- Report all new and worsening symptoms and side=-effects to your haematologist or oncologist.
- You can also contact our lymphoma nurses by clicking the contact us button at the bottom of the screen.