Overview of Peripheral T-cell Lymphoma (PTCL)
Peripheral T-cell lymphoma (PTCL) is the name given to the group of aggressive (fast growing) Non-Hodgkin lymphomas that develop when a type of white blood cell called T-cell lymphocytes become cancerous. T-cells are made in our bone marrow, but travel through our lymphatic system to our thymus where they continue to grow and develop.
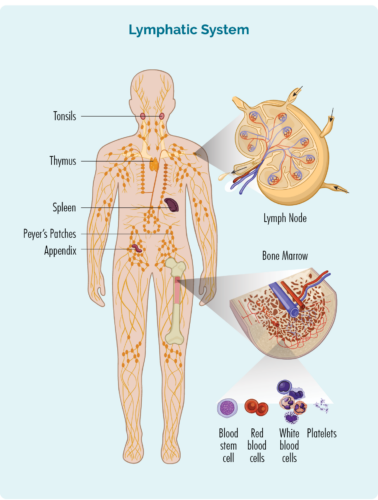
About NK cells & T-cell Lymphocytes
- Natural Killer (NK) cells are often called “NK T-cells”. They are specialised immune cells that recognise and destroy cancer cells. Unlike other T-cells, NK cells do not need to be activated to fight cancer. They are ready to fight cancer at all times, and actively move around your body on the look-out for cells that have cancerous changes.
- Other T-cells need to be activated to work effectively. They are usually resting in your thymus, lymph nodes or other parts of your lymphatic system, and only wake up and fight infection when other immune cells let them know there is an infection or disease to fight. When they wake up, T-cells can travel to any part of your body to fight the infection or disease.
- Some T-cells are responsible for “regulating” the immune response. This means that once and infection has been destroyed, the “Regulatory T-cells” tell other immune cells to “stand down” so they don’t keep fighting and cause harm to your good cells once the infection is gone.
- After fighting an infection or disease, some T-cells become “Memory T-cells” and they remember everything there is to know about the infection and how to fight it. That way, if you ever get the same infection or disease again, your immune system can fight it a lot more quickly and effectively.
T-cells and Peripheral T-cell Lymphoma (PTCL)
PTCL develops when some of your NK cells, or other T-cells become cancerous. We don’t know why this happens in some people, but we know that a change happens in your genes that provide the instructions on how the cells should grow and act. When this change happens the cells do not get the right instructions anymore, and start to develop with mutations in them that causes them to grow in an uncontrolled way, and become so mutated that they are no longer able to do their job of fighting infection and disease properly.
Peripheral T-cell lymphoma (PTCL) can affect people of any age including children, but is most common in people aged over 60 years.
For more information on how and why lymphoma develops click the link below.
Subtypes of PTCL
About 1 in 10 people with lymphoma will have a subtype of PTCL, however there are many different types of PTCL making each one very rare. While there are many different subtypes of PTCL, they can by generally classed as:
- Nodal: starting in your lymph nodes or lymphatic system
- Extra-nodal: starting outside of the lymph nodes including in your organs or skin
- Leukemic: starting in your blood or bone marrow
If you already know your subtype of PTCL and would like subtype specific information, click on the dot point below to connect to that page. If you don’t yet know your subtype, or can’t find yours below, keep reading on this page for general information on PTCL.
- Peripheral T-cell lymphoma – not otherwise specified (PTCL-NOS)
- Angioimmunoblastic T-cell lymphoma (AITL)
- Anaplastic large cell lymphoma (ALCL)
- Intestinal T-cell lymphoma
- Enteropathy-Type T-Cell Lymphoma (EATL)
- Monomorphic epitheliotropic intestinal lymphoma (MEITL)
- Nasal NK/T-Cell Lymphoma (NKTCL)
- Hepatosplenic gamma delta T-cell lymphoma
- Cutaneous T-cell Lymphoma (CTCL)
- Sezary Syndrome
- Adult T-Cell Leukaemia/Lymphoma (ATLL)
- T-cell lymphoblastic lymphoma (LL)
Patient stories
The symptoms you get can depend on the subtype of PTCL you have, and where in your body the lymphoma is. Usually, the symptom is a lump that comes up under your skin in your neck, armpit or groin that you can see or feel. This is caused by a swollen lymph node as it becomes full of cancerous lymphoma cells.
Other symptoms can include:
- Loss of appetite
- Shortness of breath
- Stomach or abdominal discomfort or pain
- Pain
- Fatigue
- Itchy skin
- B-symptoms
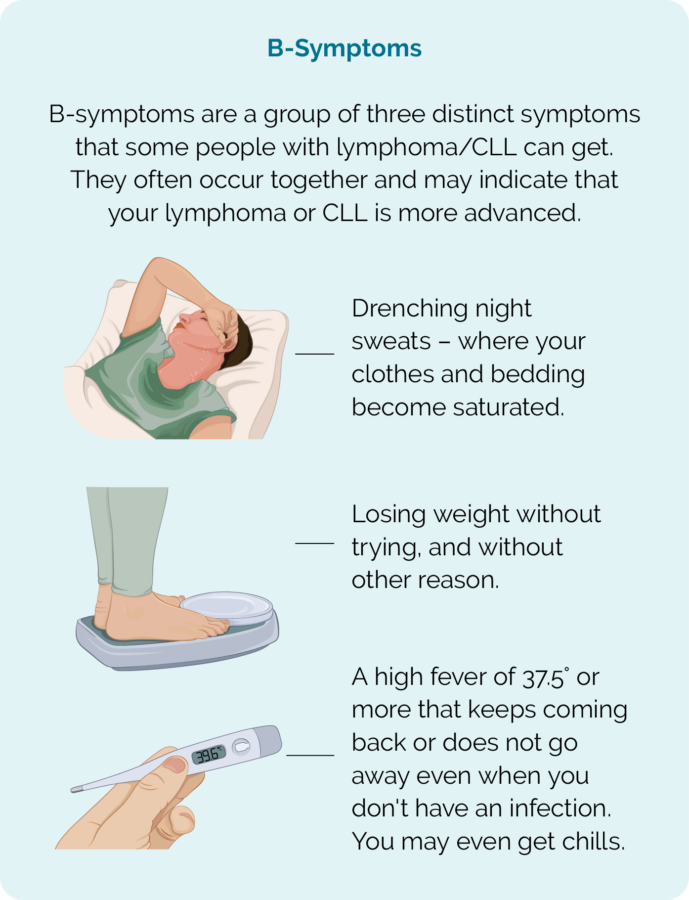
It is important to talk to your doctor about any symptoms you are getting because sometimes your symptoms can help your doctor work out the best type of treatment for you. You can find more information on symptoms of lymphoma by clicking the below link.
PTCL diagnosis, staging and grading
Diagnosing PTCL can sometimes be difficult and can take several weeks.
If your doctor thinks that you may have lymphoma, they will need to organise a number of important tests. These tests are needed to either confirm or rule out lymphoma as the cause for your symptoms. Because there are several different subtypes of PTCL, you may have extra tests to find out which one you have. This is important because the management and treatment of your subtype may be different to other subtypes of PTCL.
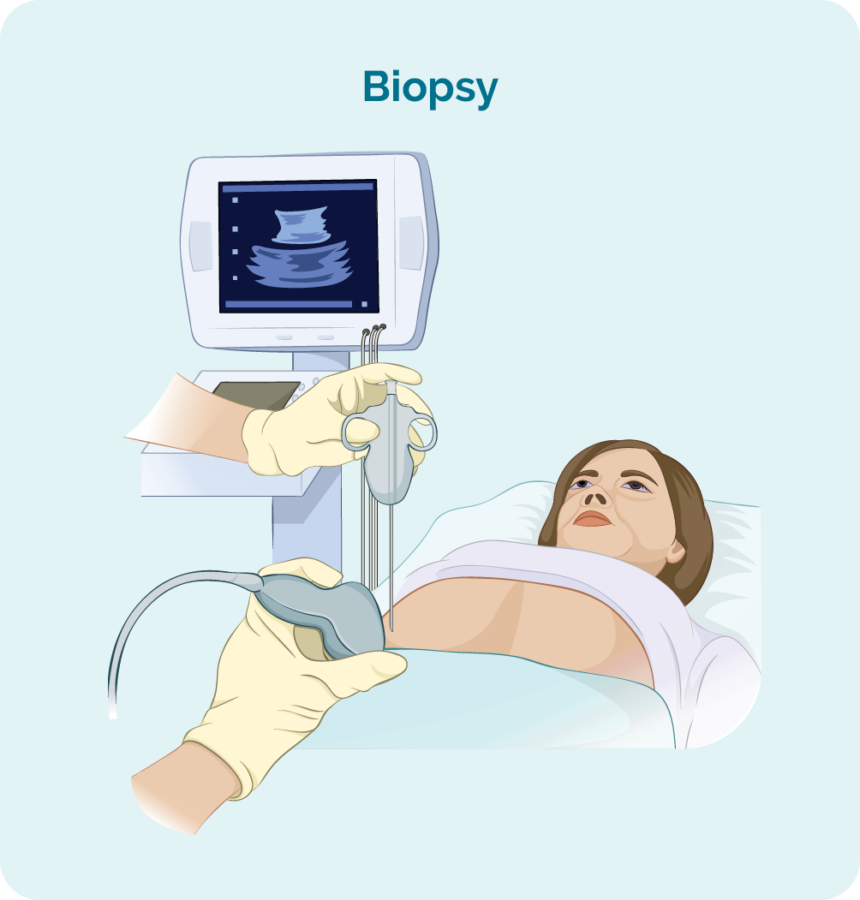
To diagnose PTCL you will need a biopsy. A biopsy is a procedure to remove part, or all of an affected lymph node and/ or a bone marrow sample. The biopsy is then checked by a scientist in pathology to see if there are changes that help the doctor diagnose PTCL.
When you have a biopsy, you may have a local or general anaesthetic. This will depend on the type of biopsy and what part of your body it is taken from. There are different types of biopsies and you may need more than one to get the best sample.
Blood tests
Blood tests are taken when trying to diagnose your lymphoma, but also throughout your treatment to make sure your organs are working properly and can cope with our treatment.
Core or fine needle biopsy
Core or fine needle biopsies are taken to remove a sample of swollen lymph node, tumour or affected skin to check for signs of PTCL.
Your doctor will usually use a local anaesthetic to numb the area so you don’t feel any pain during the procedure, but you will be awake during this biopsy. They will then put a needle into the swollen lymph node or lump and remove a sample of tissue.
If your swollen lymph node or lump is deep inside your body the biopsy may be done with the help of ultrasound or specialised x-ray (imaging) guidance.
You might have a general anaesthetic for this (which puts you to sleep for a little while). You may also have a few stitches afterwards.
Core needle biopsies take a bigger sample than a fine needle biopsy.
Excisional node biopsy
Excisional node biopsies are done when your swollen lymph node or tumour are too deep in your body to be reached by a core or fine needle biopsy. You will have a general anaesthetic which will put you to sleep for a little while so you stay still, and feel no pain.
During this procedure, the surgeon will remove the whole lymph node or lump and send it to pathology for testing.
You will have a small wound with a few stitches, and a dressing over the top.
Stitches usually stay in for 7-10 days, but your doctor or nurse will give you instruction on how to care for the dressing, and when to return to have the stitches out.
Diagnosis
Staging
Grading
Staging of peripheral T-cell lymphoma (PTCL)
Once your diagnosis of PTCL is confirmed you have more tests to see how many areas of your body are affected by the lymphoma. This is called staging.
Staging refers to how much of your body is affected by your lymphoma – or, how far it has spread from where it first started.
T-cells can travel to any part of your body. This means that lymphoma cells (the cancerous T-cells), can also travel to any part of your body. You will need to have more tests done to find this information. These tests are called staging tests and when you get results, you will find out if you have stage one (I), stage two (II), stage three (III) or stage four (IV) PTCL.
Your stage of PTCL will depend on:
- How many areas of your body have lymphoma.
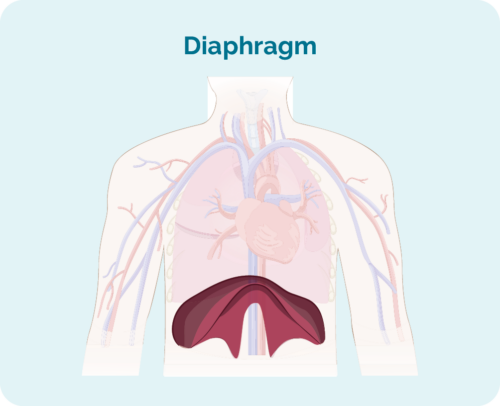
- Where the lymphoma is including if it is above, below or on both sides of your diaphragm (a large, dome-shaped muscle under the rib cage that separates the chest from your abdomen).
- Whether the lymphoma has spread to your bone marrow or other organs such as the liver, lungs, skin or bone.
Stages I and II are called ‘early or limited stage’ (involving a limited area of your body).
Stages III and IV are called ‘advanced stage’ (more widespread).
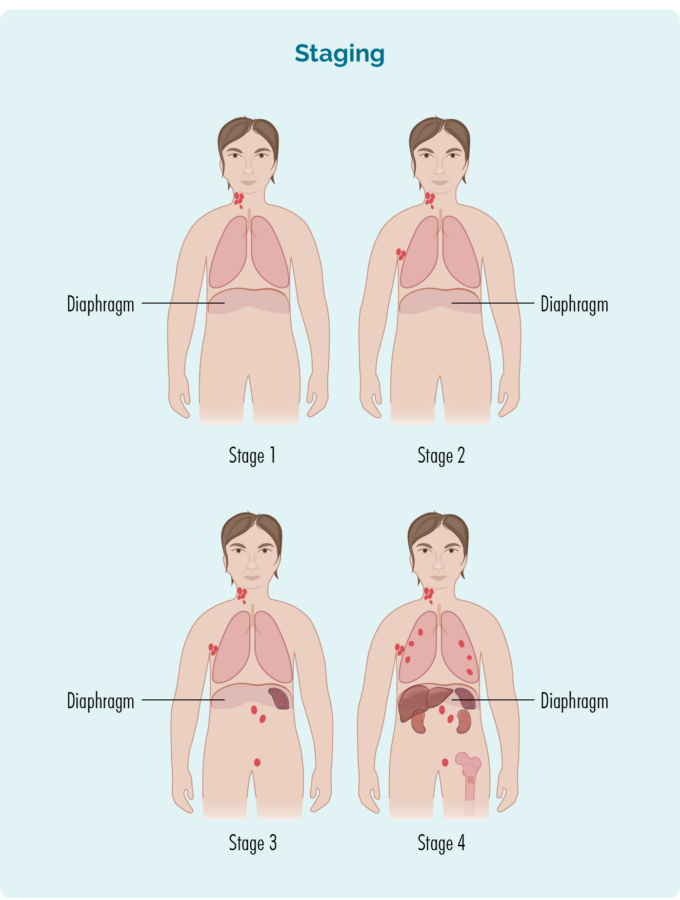
Stage 1 | one lymph node area is affected, either above or below the diaphragm* |
Stage 2 | two or more lymph node areas are affected on the same side of the diaphragm* |
Stage 3 | at least one lymph node area above and at least one lymph node area below the diaphragm* are affected |
Stage 4 | lymphoma is in multiple lymph nodes and has spread to other parts of the body (e.g. bones, lungs, liver) |
Extra staging information
Your doctor may also talk about your stage using a letter, such as A,B, E, X or S. These letters give more information about the symptoms you have or how your body is being affected by the lymphoma. All this information helps your doctor find the best treatment plan for you.
Letter | Meaning | Importance |
A or B |
|
|
E & X |
|
|
S |
|
(Your spleen is an organ in your lymphatic system that filters and cleans your blood, and is a place your B-cells rest and make antibodies) |
Tests for staging
To find out what stage you have, you may be asked to have some of the following staging tests:
Computed tomography (CT) scan
These scans takes pictures of the inside of your chest, abdomen or pelvis. They provide detailed pictures that provide more information than a standard X-ray.
Positron emission tomography (PET) scan
This is a scan that takes pictures of the inside of your whole body. You will be given and needle with some medicine that cancerous cells – such as lymphoma cells absorb. The medicine that helps the PET scan identify where the lymphoma is and the size and shape by highlighting areas with lymphoma cells. These areas are sometimes called “hot”.
Lumbar puncture
A lumbar puncture is a procedure done to check if you have any lymphoma in your central nervous system (CNS), which includes your brain, spinal cord and an area around your eyes. You will need to say very still during the procedure, so babies and children may have a general anaesthetic to put them to sleep for a little while the procedure is done. Most adults will only need a local anaesthetic for the procedure to numb the area.
Your doctor will put a needle into your back, and take out a little bit of fluid called “cerebral spinal fluid” (CSF) from around your spinal cord. CSF is a fluid that acts a bit like a shock absorber to your CNS. It also carries different proteins and infection fighting immune cells such as lymphocytes to protect your brain and spinal cord. CSF can also help drain any extra fluid you may have in your brain or around your spinal cord to prevent swelling in those areas.
The CSF sample will then be sent to pathology and checked for any signs of lymphoma.
Bone marrow biopsy
- Bone marrow aspirate (BMA): this test takes a small amount of the liquid found in the bone marrow space.
- Bone marrow aspirate trephine (BMAT): this test takes a small sample of the bone marrow tissue.
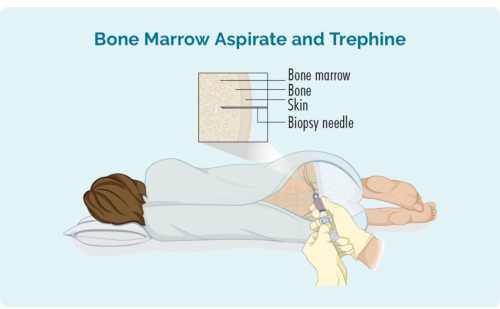
The samples are then sent to pathology where they are checked for signs of lymphoma.
The process for bone marrow biopsies can differ depending on where you are having your treatment, but will usually include a local anaesthetic to numb the area.
In some hospitals, you may be given light sedation which helps you to relax and can stop you from remembering the procedure. However many people do not need this and may instead have a “green whistle” to suck on. This green whistle has a pain killing medication in it (called Penthrox or methoxyflurane), that you use as needed throughout the procedure.
Make sure you ask your doctor what is available to make you more comfortable during the procedure, and talk to them about what you think will be the best option for you.
More information on bone marrow biopsies can be found at our webpage here.
Your lymphoma cells have a different growth pattern, and look different to normal cells. The grade of your lymphoma is how quickly your lymphoma cells are growing – whether it’s indolent or aggressive. The more aggressive your PTCL is, the more different they will look to normal cells.
The grades are Grades 1-4 (low, intermediate, high). If you have a higher grade lymphoma (more aggressive), your lymphoma cells will look the most different from normal cells, because they are growing too quickly to develop properly. An overview of the grades is below.
- G1 – low grade – your cells look close to normal, and they grow and spread slowly.
- G2 – intermediate grade – your cells are starting to look different but some normal cells exist, and they grow and spread at a moderate rate.
- G3 – high grade – your cells look fairly different with a few normal cells, and they grow and spread faster.
- G4 – high grade – your cells look most different to normal, and they grow and spread the fastest.
All this information adds to the whole picture your doctor builds to help decide the best type of the treatment for you.
It is important that you talk to your doctor about your own risk factors so you can have clear idea of what to expect from your treatments.
Treatment for peripheral T-cell lymphoma (PTCL)
Once all of the results from the biopsy and the staging scans have been completed, your doctor will review them to decide the best possible treatment for you.
Doctors take into consideration many factors about the lymphoma and the patient’s general health to decide when and what treatment is required. This is based on:
- What subtype and stage of PTCL you have.
- Any symptoms you are getting.
- How your body is being affected by the lymphoma.
- Your age.
- Your general health and wellbeing and any other conditions you are having treatment for.
- Your preferences for treatment once you have all the information needed to make an informed choice.
First-line treatment
The first time you start treatment for PTCL it is called first-line treatment. Click on the headings below to learn more about the treatment protocols.
The standard first-line treatment for PTCL may include:
- CHOP (cyclophosphamide, doxorubicin, vincristine and prednisolone)
- CHOEP (CHOP with addition of etoposide)
- BV-CHP (Brentuximab Vedotin, cyclophosphamide, doxorubicin, prednisone)
- SMILE – For NK T-cell lymphoma only (methotexate, calcium folinate, dexamethasone, etoposide, ifosphamide, mesna, GCSF, asparaginase)
- DDGP – For NK T-cell lymphoma only (dexamethasone, pegasparaginase, gemcitabine, cisplatin, GCSF)
- High-dose chemotherapy followed by autologous stem cell transplant (ASCT)
- Radiotherapy
- Clinical trial participation
Second-line and other treatments
Many people have a good response from first-line treatment and will go into remission. This where there is no detectable sign of lymphoma left in your body. But it is common for the PTCL to come back after a time in remission, this is called a relapse.
In some cases, your PTCL may not improve with the first-line treatment. If this happens, your PTCL is said to be refractory (or not responding) to treatment.
If you have refractory PTCL or have relapsed, you will need to start a different treatment. This next treatment is called second-line treatment.
Standard second-line treatments can include and of the above first-line treatments or:
- Romidepsin
- Pralatrexate
- High-dose chemotherapy followed by allogeneic stem cell transplant
- Vorinostat – For cutaneous PTCL only
- Clinical trials.
Prognosis of peripheral T-cell lymphoma (PTCL)
Prognosis is how well you are expected to respond to treatment for PTCL and what the likely outcome will be. Your prognosis is a very individual thing and depends on several things such as:
- the subtype of PTCL you have and its stage
- your age and overall health
- genetic factors that may affect treatment
- how well your body responds to the treatment
Many people respond well to treatments and go into a time of remission, but this is not the case for everyone. Some people may need several lines of treatment to get control of their disease. However, even if you get a good response early, PTCL often relapses and needs more treatment. It is important to have clear expectations about your treatment so you can plan what you need. Click on the link below for some things to consider when having treatment.
Survivorship, living with and after PTCL
A healthy lifestyle, or some positive lifestyle changes after treatment can be a great help to your recovery. There are many things you can do to help you live well with PTCL.
Many people find that after a cancer diagnosis, or treatment, that their goals and priorities in life change. Getting to know what your ‘new normal’ is can take time and be frustrating. Expectations of your family and friends may be different to yours. You may feel isolated, fatigued or any number of different emotions that can change each day.
Goals after treatment
The main goals after treatment for your PTCL is to get back to life and:
- be as active as possible in your work, family, and other life roles
- lessen the side effects and symptoms of the cancer and its treatment
- identify and manage any late side effects
- help keep you as independent as possible
- improve your quality of life and maintain good mental health
Cancer Rehabilitation
Different types of cancer rehabilitation may be recommended to you. This could mean any of a wide range of services such as:
- physical therapy, pain management
- nutritional and exercise planning
- emotional, career and financial counselling.
Summary
- Peripheral T-cell Lymphoma (PTCL) is a term used for a group rare T-cell Non-Hodgkin Lymphomas.
- PTCL happens when your T-cell lymphocytes or NK cells become cancerous.
- NK cells are specialised T-cells that are always active and ready to find and destroy cancerous cells.
- Other T-cells wait to be activated by other immune cells to fight infection and disease. There are different types of T-cells with different functions.
- T-cells can travel to any part of your body, so PTCL can also be in any part of your body.
- Symptoms of PTCL may be related to the subtype and location of your lymphoma and may include B-symptoms.
- Report all new or worsening symptoms to your doctor. They can use this information to make good decisions about your health care, including treatment options.
- PTCL may respond well to treatment, but can also be refractory or relapse after remission so you may need more than one type of treatment, at different times.
- Talk to your doctor about the expectations of your treatment.
- You are not alone, our Lymphoma Care Nurses are here to support you. You can contact them by clicking on the “Contact Us” button at the bottom of the screen.